Introduction
Falls remain one of the most common and serious health risks for older adults and those with chronic conditions, contributing significantly to injury, hospital admissions, and reduced independence.
The World Health Organization reports over 37 million falls annually severe enough to require medical attention, while 1 in 4 adults aged 65 and over in the US experience a fall each year, costing the healthcare system approximately $50 billion annually.
Most falls are preventable, yet they remain a major contributor to hospitalisations, hip fractures, and loss of independence.
On 29 April 2025, the UK National Institute for Health and Care Excellence (NICE) published its updated guideline on falls assessment and prevention (NG249).
This guideline replaces the 2013 version and reflects a broader evidence base, emphasising early identification, comprehensive assessment, and tailored interventions across clinical settings.
While the guidance is UK-specific, the themes and clinical recommendations are globally relevant, particularly for health systems focused on proactive, preventative, and person-centered care.
The overarching aim of the updated guideline is to reduce the risk and incidence of falls, and the associated consequences such as pain, injury, hospitalization, fear of falling, loss of independence, and even premature mortality.
While many recommendations reaffirm existing best practices, others represent a meaningful shift that may require service change and investment at the local level.
5 Key Focus Areas and Changes in the 2025 Guidelines
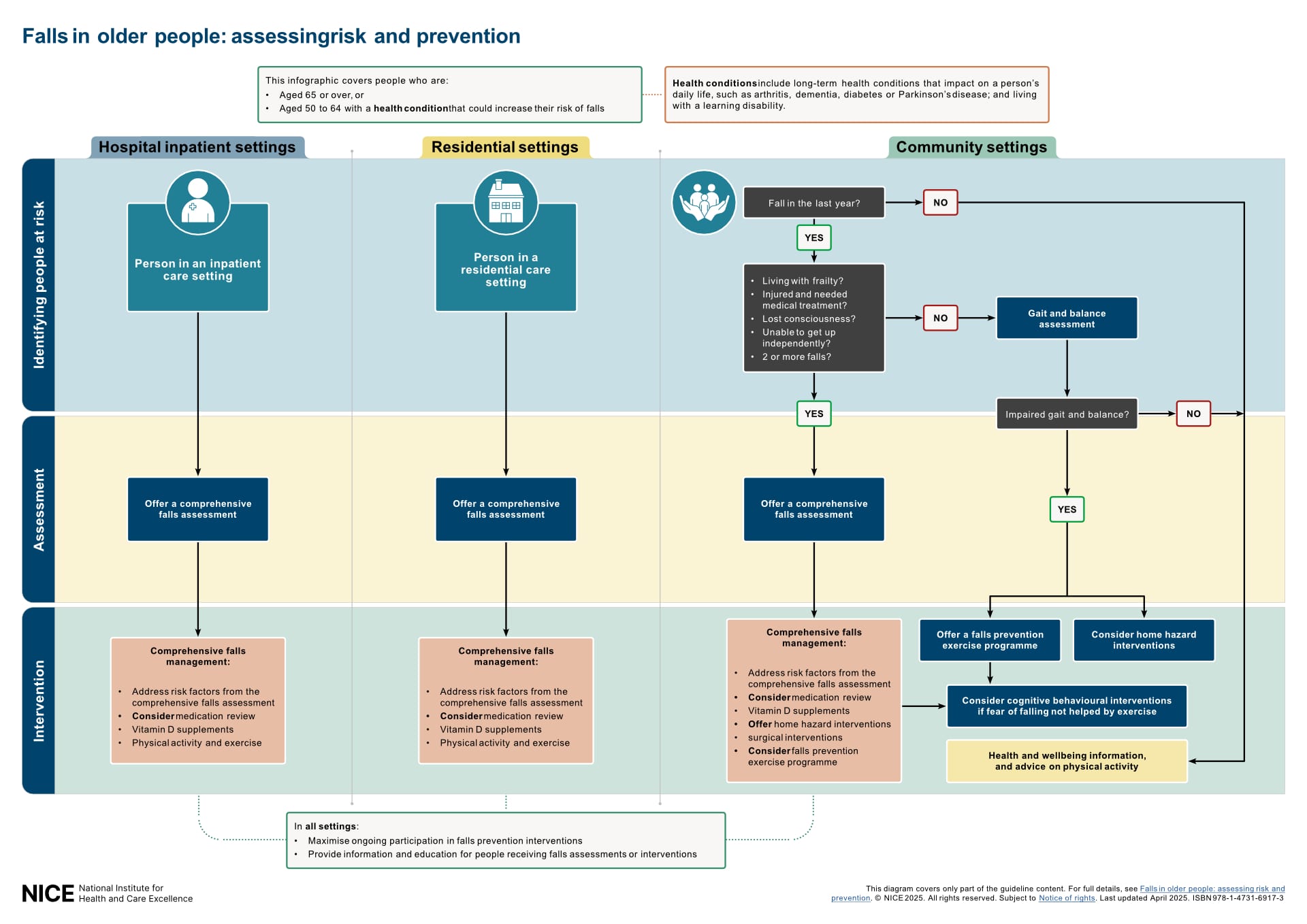
1. Expanding the Scope and Strengthening Setting-Specific Recommendations
The 2025 guideline significantly expands its scope. It now applies to people aged 50 to 64 with one or more risk factors for falls, across all care settings (including community, hospital, and residential care), where previously the guidance for this age group only applied to hospital settings.
It also formally extends its recommendations beyond the home environment to include care homes and wider community healthcare services, emphasising the need for consistent, system-wide approaches to falls prevention.
Community Settings:
- Individuals aged 50 and over who have fallen in the past year and meet specific risk criteria should receive a comprehensive falls assessment.
- For those requiring comprehensive falls management, the guideline recommends conducting home hazard assessments using validated tools (Recommendation 1.3.5).
Hospital Inpatient Settings:
- All inpatients aged 65 and over, or those at increased risk due to factors such as frailty or a history of falls, should be considered at risk and routinely receive comprehensive falls assessments and tailored interventions.
- In addition, setting-specific education should be provided on fall risks, safe mobility, equipment use, and how to seek help during a hospital admission (Recommendation 1.5.2).
Residential Care Settings:
- All residents should be considered at increased risk and offered both comprehensive assessment and personalized falls management, recognizing the higher baseline prevalence of frailty and multimorbidity in this population.
- Residents should also be supported with information on staying active, managing safety concerns, using equipment appropriately, and involving carers or visitors in identifying potential hazards (Recommendation 1.5.3).
The 2025 guideline also places greater emphasis on strengthening education and communication across all care settings.
Recommendation 1.5.1 outlines the importance of providing individuals (and where appropriate, their families or carers) with tailored information on falls risk, modifiable risk factors, effective interventions, and what to do if a fall occurs.
2. Emphasising Early Identification of At-Risk Individuals
The updated recommendations support early identification of individuals at risk (see Comprehensive Falls Assessment below), including those who:
- Have fallen in the past year
- Are living with frailty
- Have sustained injuries or experienced loss of consciousness during a fall
- Were unable to get up independently following a fall
- Have had multiple falls
3. Personalising and Broadening Risk Assessments and Tailoring Interventions
Risk assessments should be tailored to the individual (see Comprehensive Falls Assessment below), considering:
- Physical and cognitive health
- Home and care environment
- Balance, gait, dizziness, and mobility
- Medication use and underlying conditions such as diabetes, Parkinson’s disease, or cardiovascular issues
Where appropriate, occupational therapists should lead home hazard assessments (Recommendation 1.3.6), supported by other trained professionals or supervised staff.
Based on the assessment findings, interventions should be selected and adapted to each person’s risk profile and preferences (see Comprehensive Falls Management below).
These may include home hazard modification, physiotherapy, strength and balance training, cognitive behavioural approaches for fear of falling, or the use of assistive technologies where appropriate.
4. Clarifying the Role of Falls Risk Prediction Tools
The 2025 NICE guideline (Recommendation 1.1.1) advises against the use of standalone falls risk prediction tools to estimate a person’s likelihood of falling.
Evidence shows that tools based solely on single measures lack sufficient accuracy (i.e. sensitivity or specificity <0.7) when used in isolation and do not reflect the multifactorial nature of falls risk.
As these tools often categorize individuals into broad risk levels without informing specific interventions, the guideline concludes they may distract from more effective, personalized approaches to care.
Nonetheless, the committee notes that assessments such as balance tests, strength measures, and functional mobility evaluations are clinically useful when used as part of a Comprehensive Falls Assessment.
The guideline recommends:
- Prioritising clinical judgement and case finding, particularly in individuals with a history of falls, frailty, or observed balance and mobility issues
- Using comprehensive assessments that evaluate multiple domains, including physical health, cognitive status, environment, and medication use
- Recognising the potential of wearable technologies, while highlighting the current lack of sufficient real-world evidence to support their predictive use
5. Expanding Access to Exercise and Physical Activity
The updated guideline maintains support for evidence-based falls prevention exercise programmes in the community.
Notably, it now emphasises improving access to exercise interventions for people even if they do not require a full assessment, encouraging widespread participation in activity as a preventive measure.
It recommends that older adults, including those in hospitals or care homes, are encouraged to remain active unless medically contraindicated.
New guidance (Recommendation 1.4.1) also emphasises the importance of maximising participation by agreeing achievable goals, addressing barriers, offering flexible and supervised delivery formats (individual or group), and encouraging social connection where possible.
Source: NICE (NG249)
Comprehensive Falls Assessment
Linked to Quality Standard QS86; Statement 2
A comprehensive falls assessment aims to identify a person’s individual risk factors for falling and should guide tailored, evidence-based interventions.
While often delivered by a specialist falls service, the assessment can also be conducted in primary care, community teams, or outpatient settings, by either a single trained professional or a multidisciplinary team.
Who qualifies for a comprehensive falls assessment?
People aged 50+ who:
- Have one or more risk factors (e.g. frailty, long-term conditions, recent stroke or cognitive impairment)
and - Have fallen in the past year and meet any of the following criteria:
- Sustained injury requiring medical or surgical care
- Experienced loss of consciousness
- Were unable to get up independently
- Had two or more falls in the last year
- Are hospital inpatients or residents in care homes
What does the assessment include?
The assessment should be tailored to the individual and may include:
Physical and Functional Health
- Gait, balance, mobility, and muscle strength (e.g. grip strength, TUG, gait speed)
- Cardiovascular checks (including postural blood pressure)
- Neurological examination
- Osteoporosis risk assessment
- Footwear and foot condition
- Visual and hearing impairments
- Urinary continence
Cognitive, Mood, and Behavioural Factors
- Cognitive function and mood
- Delirium screening (in hospitals and residential care settings)
- Alcohol misuse assessment
- Fear of falling and perceived functional ability
Medication and Medical History
- Comprehensive medication review
- Review of long-term conditions (e.g. Parkinson’s disease, dementia, diabetes, arthritis)
- Nutritional status, hydration, and weight loss
Environmental and Lifestyle Factors
- Dizziness and vertigo evaluation
- Assessment of home and care environment
- Evaluation of physical activity levels
The findings from the comprehensive falls assessment should directly inform the development of a personalized management plan.
Comprehensive Falls Management
Linked to Quality Standard QS86; Statement 3
A comprehensive falls assessment allows a person’s risk factors to be identified.
If the comprehensive assessment identifies risk factors, individuals should receive comprehensive falls management interventions tailored to their needs (Recommendations. 1.3.1-1.3.25).
This applies across all care settings, including hospital, community, and residential care.
Who requires comprehensive falls management?
People aged 50+ who meet one or more of the following criteria:
- Have fallen in the past year and:
- Live with frailty
- Sustained injury requiring medical/surgical care
- Experienced loss of consciousness
- Were unable to get up independently
- Had two or more falls in the past year
- Are hospital inpatients or residents in care settings
Risk factors may include long-term conditions such as Parkinson’s disease, dementia, diabetes, arthritis, stroke, and learning disabilities.
Core components of comprehensive falls management:
Clinical Interventions
- Advice on vitamin D and bone health
- Surgical interventions (e.g. cataracts, cardiac pacing)
- Structured medication review, especially for psychotropic drugs
- Clinicians are advised to review medications that may increase fall risk (e.g., sedatives, antihypertensives) and adjust prescriptions where appropriate to reduce risk.
Functional and Environmental Support
- Access to evidence-based exercise programmes (e.g. strength and balance training)
- Home hazard assessments and modifications
- Occupational therapist-led interventions are preferred for effectiveness and cost-efficiency, though trained staff may also deliver these under supervision
Psychosocial Support and Lifestyle Guidance
- Cognitive behavioural approaches to address fear of falling
- Personalised advice on physical activity and mobility strategies
NICE Quality Standards: Measuring the Delivery of Best Practice in Falls Prevention
While guidelines describe how care should be delivered, quality standards define how performance should be measured. Each quality standard consists of a concise, high-priority statement designed to drive measurable improvement in care quality and consistency across settings.
Updated in April 2025 (QS86) to reflect the revised NICE guideline on Falls, these statements emphasise early identification, personalised assessment, and targeted intervention across all care settings, highlighting the importance of making every contact count in addressing falls risk.
Statement 1: Asking About Falls History
People aged 50 to 64 with one or more risk factors for falls, and people aged 65 or over, are asked about the details of any falls when they attend appointments or assessments in community or hospital settings. [2017, updated 2025]
- A recent history of falls is the strongest predictor of future falls, and routine enquiry enables timely identification of those at risk.
Statement 2: Comprehensive Falls Assessment
People aged 50 to 64 with 1 or more factors that could increase their risk of falls and people aged 65 or over have a comprehensive falls assessment if they meet the criteria for a comprehensive falls assessment. [2017, updated 2025]
- The assessment should be multi-factorial and personalised, taking place in settings with the appropriate clinical expertise and governance.
Statement 3: Tailored Falls Management
People aged 50 to 64 with 1 or more factors that could increase their risk of falls and people aged 65 or over have tailored interventions that address their individual risk factors if they need comprehensive falls management to reduce their risk of falling. [2017, updated 2025]
- These may include medication review, home hazard modification, exercise, or referral to specialist care.
Statement 4: Initial In-Hospital Response
People who fall during a hospital stay are checked for signs or symptoms of fracture and potential spinal injury before being moved. [2015]
- This prevents further harm from inappropriate handling and ensures timely escalation where needed.
Statement 5: Safe Manual Handling in Hospital
People who fall in hospital and show signs of fracture or spinal injury are moved using safe manual handling methods. [2015]
- This protects both the patient and the staff involved in the transfer.
Statement 6: Post-Fall Medical Examination
People who fall during a hospital stay receive a medical examination. [2015]
- This ensures that the cause and impact of the fall are identified and managed appropriately.
What This Means for Health Systems and Providers
The updated 2025 NICE guidelines reaffirm that falls prevention is not a one-size-fits-all intervention. It requires individualised care, cross-setting consistency, and clinical judgement.
These recommendations align with a global shift toward proactive, personalized preventative care.
For healthcare systems facing the dual pressures of ageing populations and chronic disease, effective falls screening and intervention are essential to maintaining independence, reducing emergency admissions, and controlling long-term costs.
Care organizations in the UK and internationally, across primary care, hospitals, home health, or senior living settings, can use the NICE guidelines as a framework to:
- Expand prevention efforts to include at-risk adults aged 50-64, not just those 65 and over.
- Standardise screening and assessment approaches across community, hospital, and residential care settings.
- Implement evidence-based interventions tailored to individuals’ risk factors and care environments.
- Optimise resource use by aligning service delivery models with local capacity and needs.
- Enhance care coordination by enabling multidisciplinary collaboration and better continuity across settings.
Able Assess Falls Risk Screening
The updated guidelines underscore the need to replace predictive tools with clinically meaningful assessments that can guide personalized, evidence-based interventions.
This principle underpins the design of Able Assess, a platform built to support real-world implementation of the NICE recommendations by enabling reliable, scalable, and low-cost falls risk assessments across care settings.
Able Assess integrates four validated functional measures: grip strength, gait speed, balance, and mobility, into a structured, multi-domain assessment framework that can be completed in under five minutes.
This enables efficient, objective, and scalable evidence-based decision-making without relying on single-metric risk prediction.
To learn more or discuss how Able Assess could support your organization, visit our website or get in touch.

